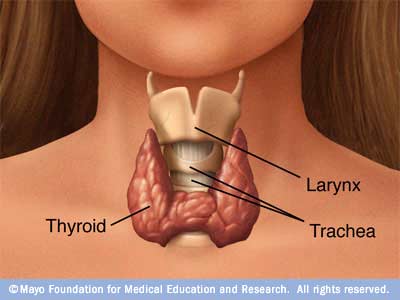
Several studies show a strong link between autoimmune thyroid disease (both Hashimoto’s and Graves’) and gluten intolerance.
The link is so well established that researchers suggest all people with autoimmune thyroid disease (AITD) be screened for gluten intolerance, and vice versa. Why is there a connection? It’s a case of mistaken identity.
The molecular structure of gliadin, the protein portion of gluten, closely resembles that of the thyroid gland.
When gliadin breaches the protective barrier of the gut, and enters the bloodstream, the immune system tags it for destruction. These antibodies to gliadin also cause the body to attack thyroid tissue. This means if you have AITD and you eat foods containing gluten, your immune system will attack your thyroid. Even worse, the immune response to gluten can last up to 6 months each time you eat it. This explains why it is critical to eliminate gluten completely from your diet if you have AITD.
There’s no “80/20″ rule when it comes to gluten.
Being “mostly” gluten-free isn’t going to cut it. If you are gluten intolerant, you have to be 100% gluten-free to prevent immune destruction of your thyroid.
So how do you find out if you are gluten intolerant?
Unfortunately, standard lab tests aren’t very accurate. The only reliable test for gluten intolerance is a “gluten challenge.” This involves removing gluten from the diet completely for a period of at least 30 days (though preferably three months), and then adding it back in after that. If symptoms improve during the elimination period, and return when gluten is reintroduced, a diagnosis of gluten intolerance can be made. However, for many people a gluten-free diet isn’t enough. Some grains that don’t contain gluten, such as corn, oats and rice, contain proteins that are similar enough in structure to gluten to elicit an immune response in people with celiac disease or gluten intolerance. Approximately 50% of people with Celiac are also intolerant to casein a protein found in Dairy products.
The most effective way we have found is for our patients to go on our
Purification Program and re-introduce foods in a step by step format with supervision.
Unfortunately, standard lab tests aren’t very accurate. They test for antibodies to gluten in the bloodstream. But antibodies in the blood will only be found in cases where the gut has become so permeable that gluten can pass through. The only reliable test for gluten intolerance is a “gluten challenge.” This involves removing gluten from the diet completely for a period of at least 30 days (though preferably three months), and then adding it back in after that. If symptoms improve during the elimination period, and return when gluten is reintroduced, a diagnosis of gluten intolerance can be made. However, for many people a gluten-free diet isn’t enough. Some grains that don’t contain gluten, such as corn, oats and rice, contain proteins that are similar enough in structure to gluten to elicit an immune response in people with celiac disease or gluten intolerance. Moreover, about 50 percent of patients with celiac disease show signs of intolerance to casein (the protein in milk), and up to 30 percent of celiac disease patients continue to have symptoms or clinical signs after adopting a gluten-free diet.
One reason gluten intolerance goes undetected in so many cases is that both doctors and patients mistakenly believe it only causes digestive problems. But gluten intolerance can also present with inflammation in the joints, skin, respiratory tract and brain
. The short version: foods that contain gluten (both whole grains and flours) often also contain substances that inhibit nutrient absorption, damage our intestinal lining, and activate a potentially destructive autoimmune response. The good news is that if you have AITD and are gluten intolerant removing gluten completely from your diet will dramatically improve your health. It’s not easy, but it’s worth it.