Why you should think twice about a C section
August 22, 2015
The number of moms having C sections today versus a few years ago has increased dramatically. I am not talking about life saving C sections but those that are steeled as elective surgery…
Below is some recent research to consider
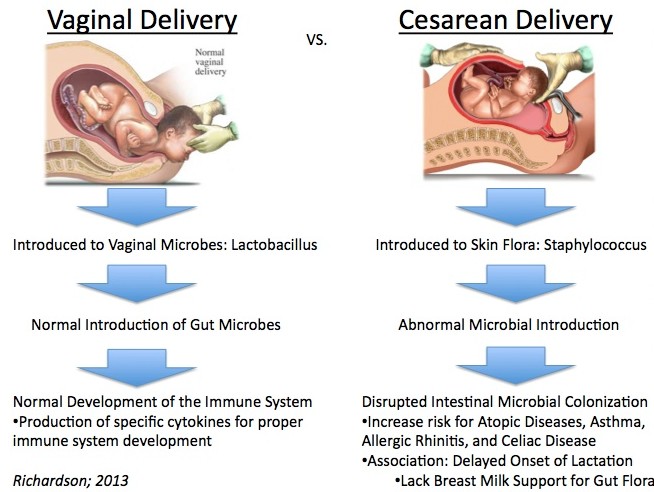
A fecal sample analysis of 98 Swedish infants over the first year of life found a connection between the development of a child’s gut micro biome and the way he or she is delivered. Babies born via C-section had gut bacteria that showed significantly less resemblance to their mothers compared to those that were delivered vaginally.
The study, which appears May 11 in Cell Host & Microbe’s special issue on “The Host-Microbiota Balance,” also found nutrition to be a main driver of infant gut microbiome development–specifically the decision to breast-feed or bottle-feed.
Gut bacteria are suspected to be a source of nutrients and vitamins for a growing infant. Our intestinal tenants are able to interact with normal cellular processes to, for example, produce essential amino acids. Understanding the role individual gut microbes play in metabolism, immunity, and even behavior is an active area of investigation.
This new study, led by Bäckhed and Jovanna Dahlgren at the University of Gothenburg, Sweden, and Wang Jun at the Beijing Genomics Institute-Shenzhen, China, supports previous observations that most early bacterial colonizers of the gut are derived from the mother. The investigators noted that while C-section babies receive less of their mother’s microbes, they are still able to be passed on through the skin and mouth.
Once bacteria take hold in an infant’s gut, their populations shift depending on what a child eats.
The researchers believe that the cessation of breast-feeding is such a significant moment in microbiome development because certain types of bacteria thrive on the nutrients breast milk provides. Once these nutrients are no longer available, other bacteria emerge that are more commonly seen in adults.
“Our results underscore the role of breast-feeding in the shaping and succession of gut microbial communities during the first year of life,” the authors write. “The gut microbiota of children no longer breast-fed was enriched in species belonging to Clostridia that are prevalent in adults, such as Roseburia, Clostrium, and Anaerostipes. In contrast, Bifidobacterium and Lactobacillus still dominated the gut microbiota of breast-fed infants at 12 months.”
The Infant Gut and Antibiotics: Long-Term Effects
Antibiotics account for one quarter of all medications given to children, with a third of prescriptions considered unnecessary. In addition to concerns about antibiotic resistance, these drugs are known to disrupt a child’s gut microbiome in ways that a growing amount of evidence suggests may have long-term consequences, including obesity, allergies, and autoimmune diseases.
Based on a review of the literature, biotechnologist Dan Knights, of the University of Minnesota, and colleagues developed a framework for how antibiotics may be acting in the gut to cause these outcomes. In the case of allergies, for example, the use of antibiotics may eradicate key gut bacteria that help immune cells mature. These cells would have been essential for keeping the immune system at bay when confronted with allergens. Even if these bacteria return, the immune system remains impaired.
“The framework presented here links together the existing epidemiological and mechanistic studies on antibiotics and various gut-mediated disease outcomes,” the authors write. “Large, integrated studies designed to focus on short- and long-term impact of antibiotics, in terms of both microbiome composition and disease risk, with careful consideration of the factors presented here, will be critical as we move toward an increased understanding of related disease etiologies.”
The researchers also developed a diagnostic test that can calculate the developmental age of a baby’s gut microbiome relative to healthy babies. A similar test could be used by pediatricians to identify and potentially treat infants more than a month behind normal development.
The Gut Microbiome’s Role in Asthma
The search for answers in the medical mystery around the recent increase in asthma prevalence, especially for children up to age four, has led researchers to consider changes in the gut and airway microbiome as a contributing environmental factor in the development of this treatable, but uncomfortable, condition.
Susan Lynch and Kei E. Fujimura of the University of California San Francisco present the latest research in mice exploring this relationship, especially how specific types of bacteria alter the presence of different immune cells. Though still an emerging body of work, they believe it is evidence that manipulation of the airway/gut microbiome at an early age could lead to new strategies to prevent or manage asthma.
Story Source:
The above post is reprinted from materials provided by Cell Press. Note: Materials may be edited for content and length.
Journal References:
Bäckhed et al. Dynamics and Stabilization of the Human Gut Microbiome during the First Year of Life. Cell Host & Microbe, May 2015 DOI: 10.1016/j.chom.2015.04.004
Vangay et al. Antibiotics, Pediatric Dysbiosis, and Disease. Cell Host & Microbe, May 2015 DOI: 10.1016/j.chom.2015.04.006
Fujimura et al. Microbiota in Allergy and Asthma and the Emerging Relationship with the Gut Microbiome. Cell Host & Microbe, May 2015 DOI: 10.1016/j.chom.2015.04.007
Cite This Page: